AI/ML/NLP
Artificial intelligence and machine learning promise to improve the efficiency of healthcare and to reshape healthcare. However, there are two central challenges to the broad dissemination fo AI in healthcare. First, AI should be subject to rigorous evaluation to ensure that it improves patient outcomes, not just statistical metrics. Second, AI is only as good as the data it is based on. Biased data and data collection can lead to biased results. At HTI, we focus on developing and rigorous implementation of AI in clinical and policy settings, and developing methodologies to identify and mitigate bias in AI.
Behavioral Economics and Cost Control
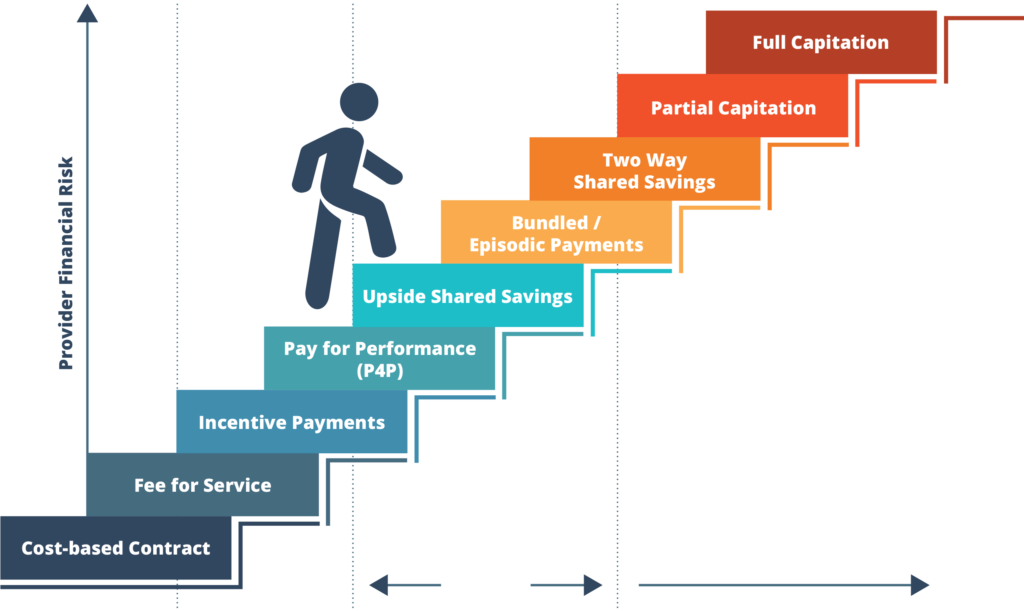
Behavioral economics provides insights about the delivery of effective incentives, information, and infrastructure to facilitate the delivery of high-value care. It suggests that the structure and delivery of incentives, delivery and timing of information, and re-design of infrastructure can shape behavior. At HTI, we work to incorporate behavioral economics principles into our collaborations with payers and providers to create interventions that can drive quantifiable changes in physician behavior and savings.
Projects
|
Behavioral Economics
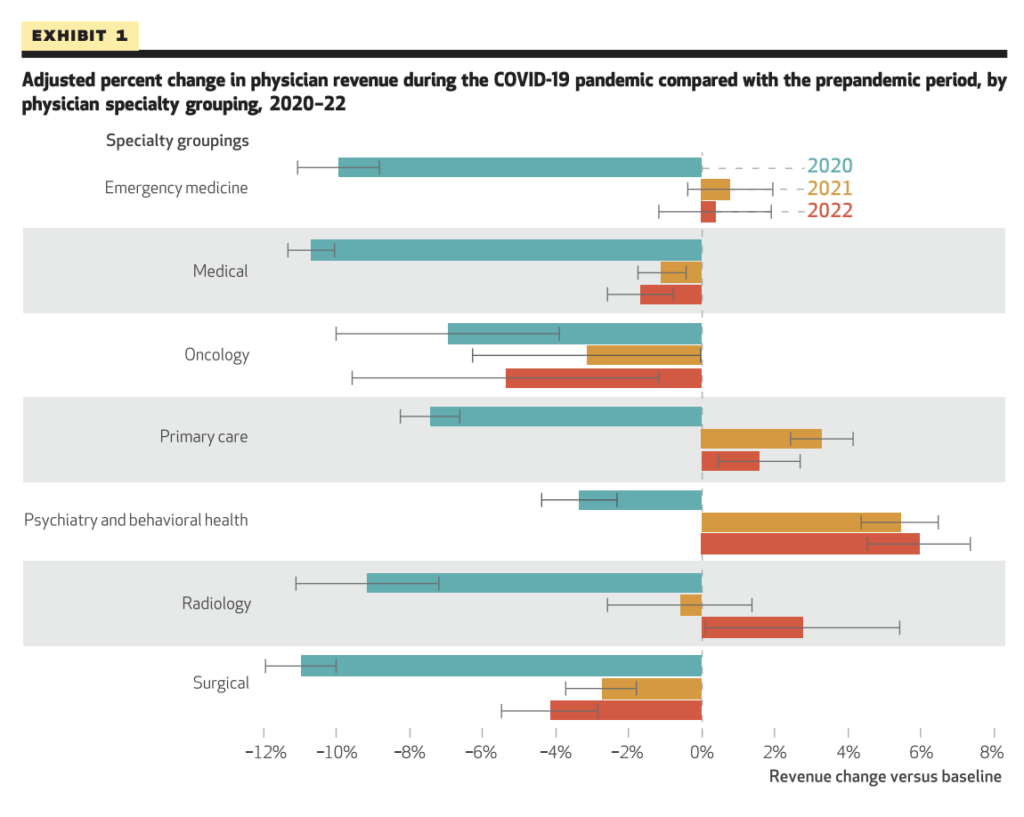
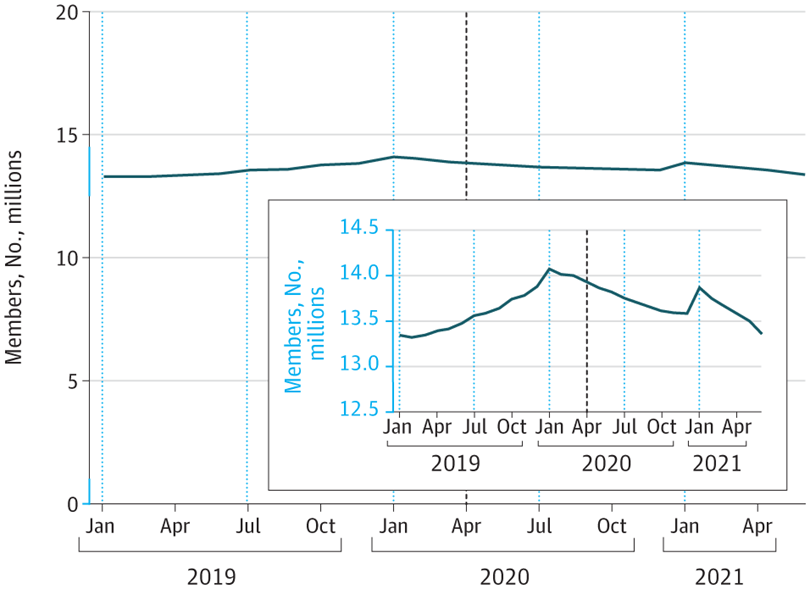
Covid
HTI is investigating some of the most pressing concerns raised by COVID-19. COVID-related shifts in healthcare have led to unforeseen outcomes in spending, utilization, and care patterns. Covid has also exacerbated health disparities both domestically and abroad. HTI leaders have risen to the highest level of influence nationally and internationally to act as trusted sources of sound policy and ethical guidance to local and state policymakers.
Academic / Publications
|
COVID
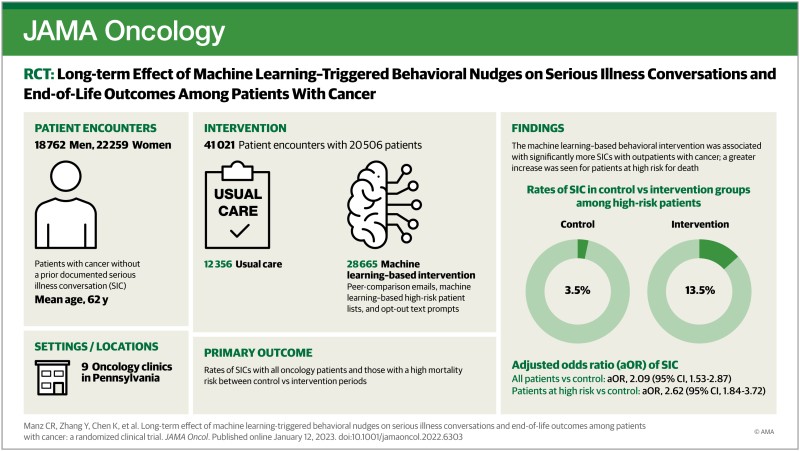
End of Life Care
End of life care constitutes about 10% of total US health care spending and approximatley 25% of all Medicare spending. At $80,000 per patient, the US has the highest mean per capita expenditures in the last 12 months of life in the world, along with the highest number of hospitalizations and intensive care unit admissions. Much of this care is not concordant with patients’ wishes near the end of life.
Hospice has not consistently reduced costs at the end of life. Early specialty palliative care has been shown to improve patient quality of life and symptoms and has held promises of large health savings mainly through the avoidance of utilization, namely hospitalization and ED visits at the end of life.
Academic / Publications
|
End of Life
Academic / Publications
|
End of Life
Academic / Publications
|
End of Life / Machine Learning
Hospital & Specialty Care
Projects
|
Hospital & Specialty Care
Projects
|
Hospital & Specialty Care
Primary Care and Population Health
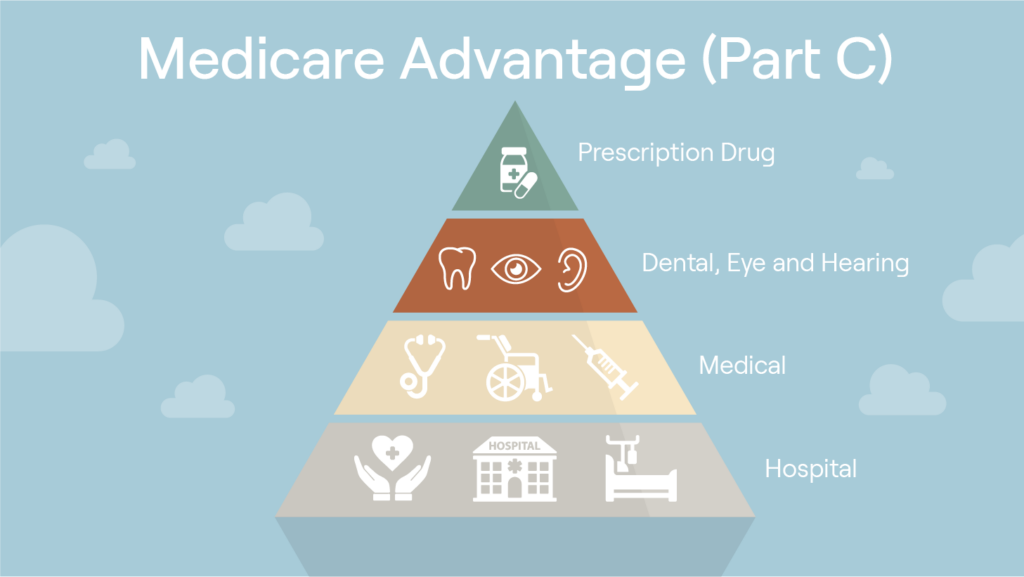
Population health has emerged as a key component of health care and public health innovation. Primary care providers are uniquely positioned to support communities in improving population health outcomes, while also engaging in each patient’s care processes and journeys. Innovative population health programs have begun to drive previously siloed topic areas into a clearer integrated landscape in which health is seen as part of a holistic model, encompassing all potential social determinants. Empowering primary care providers to drive improvements in population health is a promising avenue. Collaboration involving population health and primary care within research, policy-making, and intervention development creates exciting new visions of how a society can care for its communities and catalyze change through system and delivery models.
HTI recognizes the uniquely powerful potential primary care providers hold to greatly improve outcomes among their patients, and is collaborating with insurers to revolutionize the way we incentivize and design payments for primary care providers.
Projects
|
Primary Care and Population Health